Green nephrology
Review of the Haemodialysis processes in a single satellite dialysis unit
By: Leeds Teaching Hospitals NHS Trust
Potential to save 15,828kgCO2e and £33,435.33 per year if changes implemented in all 8 of Leeds dialysis units.
£2,837.05 (Actual)
1,914.4 kgCO2e (Actual)
Team members:
- Jemma Alison Hardy – Satellite Dialysis Unit Sister
- Peter Jones – Renal Technical Services Manager
- Terence Simpson – Renal Technologist
- Dr V R Latha Gullapudi - Consultant Nephrologist
- Dr Mark Wright- Consultant Nephrologist and Haemodialysis Lead
Aims:
- Reducing the number of disinfections of the dialysis machines to once in 24 hrs in staggered manner and replacing the others with rinsing process
- Once the initial priming process of the dialysis machines is complete, placing them standby mode whilst waiting to connect patients to the machine
- Reducing the number of pharmacy deliveries from weekly to biweekly to the satellite dialysis unit
Background:
Haemodialysis is lifesaving therapy for patients with kidney failure. However, it comes with huge environmental costs as it involves usage of vast amount of medical consumables, water, and electricity. It is estimated that 3.8 tonnes of carbon-dioxide equivalent emissions are produced by one patient’s dialysis treatment per year (1). In the unit under review, we provide services to our patients in two different shifts per day. This means that a single dialysis machine is routinely used for provision of two dialysis treatments in a 24 hour period. Dialysis machines are primed and turned on at the beginning of the day, meaning dialysis fluid runs continuously whilst waiting for the patients to be connected. Each dialysis machine gets three heat disinfections per day.
Methods:
We started by creating a process map of the steps from the production of dialysis fluid to use of dialysis machine to identify our aims as above. We discussed aims 1 and 2 with the other staff members on the unit during the daily handovers. The majority of staff were enthusiastic to try the suggested changes which supported embedding these changes into everyday routines. A similar approach was adopted for Aim 3 by seeking staff opinions, exploring the availability of storage space, rearranging storage cupboards to improve utilisation of the available space, and relabelling of the cupboards as per the new agreed storage arrangements.
Measurement:
Baseline data was collected on
- Aim 1: electricity and water usage with each episode of disinfection and rinse during 24 hour periods for one dialysis machine. We then projected the electricity and water use over one year.
- Aim 2: the average waiting times between the dialysis machined being primed and turned on, to when a patient was connected. We then measured the consumption of electricity, water and central acid usage during this waiting time per minute and projected it over a: one-year period. There is a scope for further savings from this change by reduced number of central acid deliveries, however it is not possible to precisely calculate at this stage.
- Aim 3: Reducing pharmacy deliveries from weekly to biweekly will lead to an average saving of 104 miles in transportation per year. We are liaising with the teams at the other satellite units within the Trust to investigate if the same change is feasible in their setting. This would yield higher milage savings.
Results:
In total, changes implemented will save 1,914.4 kgCO2e and £2,837.05.
- electricity: 1,672.3kgCO2e and £1,285.90
- water: 41.8kgCO2e and £264.90
- travel (miles): 9.8kgCO2e and £58.24
- acid savings: 190.3kgCO2e and £1,228.00
This satellite unit is a part of Leeds Haemodialysis services which currently provides care provision for 550 incentre dialysis patients in 8 different dialysis units. After taking into consideration of the shift patterns in each unit, if we implement aims 1 and 2 across our haemodialysis services, the estimated savings will be much higher, with 15,828kgCO2e and £33,435.33 saved per year.
If the same small changes were possible for all 24,365 people receiving dialysis in the UK2 and energy consumption of all dialysis equipment was similar across the 70 renal centres in the UK, the national reduction in CO2 emissions could be in the region of 4,495kg per treatment session. If everyone was having dialysis thrice per week, that would reduce CO2 emissions by approximately 700 tonnes per year. Social sustainability and clinical outcomes: The proposed changes may not directly impact individual patient experience but may contribute to an improvement in the turnaround of the patients in the dialysis unit, for example from saving time by replacement of disinfection (40 minutes) with rinse (9 minutes) of the machine in between patients. The unit is planning to move from a 2 shift to 3 shift cycle. Our new system will support in reduce staff workload.
Steps taken to ensure lasting change and conclusion:
We were pleasantly surprised by how much we could reduce our central acid water and electricity consumptions with relatively simple changes. Meeting with colleagues regularly and tackling a different sort of problem to usual was really uplifting and motivating, especially when we realised how much potential benefit there would be when we roll out across the service. Our next steps are to spread this enthusiasm by sharing our project aims and finding at an upcoming departmental meeting, and to explore if the other satellite units would consider a reduction in their pharmacy deliveries.
We are continuing to explore options for additional projects
- Aim 4: Water wastage from the purification process and system was measured as 1,337,000 litres/ year. Across the service equates to approximately 16,848,000 L of water wasted per year (equivalent to 6 Olympic sized swimming pools). We are liaising with appropriate teams to enable redirection of this water to grey water systems of our healthcare setting. Significant progress has been made in one of our other satellite dialysis units and we are looking forward to continuing this work to maximise the benefit of water preservation.
- Aim 5: We use acid supplied in 6 litre plastic canisters and our standard practice is to use one canister for each patient/ treatment. The leftover acid goes down the drain systems. On measurement of the wastage of the acid, the cumulative wastage of acid comes down to 18.75 Litres over 10 dialysis treatments. We are currently exploring the feasibility of avoiding this wastage, by liaising with the infection control team regarding potential safety issues if we were to use a cannister for multiple patients.
- Aim 6: Currently we do not recycle the plastic acid canisters. We are in discussion with the hospital wastage management team regarding recycling potential of these canisters by using existing steri-melt facilities.
References:
- Connor A, Lillywhite R, Cooke MW. The carbon footprints of home and in-center maintenance hemodialysis in the United Kingdom. Hemodial Int. 2011 Jan;15(1):39-51. doi: 10.1111/j.1542-4758.2010.00523.x. Epub 2011 Jan 14. PMID: 21231998.
- UK Renal Registry (2021) 23rd Annual Report- data to 31/12/2019, Bristol, UK. Available from renal.org/audit-research/annual-report
Leeds Teaching Hospitals NHS Trust - Haemodialysis
Project developed as part of the 2022 Leeds Green Ward Competition. Full impact report available at Green Ward Competition | Centre for Sustainable Healthcare.
Changing the 3 monthly blood test postage kits for patients on the renal transplant register
By: Leeds Teaching Hospitals NHS Trust
Please see social sustainability and clinical and health outcomes sections below
£1951.38 (Actual)
1219.9 kgCO2e (Actual)
Team members:
- Natalie Bird - Clinical Nurse Specialist, Renal Transplant
- Laura Kirk - Clinical Nurse Specialist, Renal Transplant
- Jo Wales - Clinical Nurse Specialist, Live Renal Donation
- Jo Hitchings - Senior Clinical Support Worker
Project aims:
To measure the environmental, social and financial benefits of a new postal system compared with an old postal system.
Background:
Patients active on the transplant register and those listed for simultaneous kidney and pancreas transplant must have regular blood tests (every 1-3 months) to re-examine their antibodies. With patients all over the region, transporting these samples to the laboratory can be logistically challenging and expensive.
As a team, the renal transplant department is already very proactive in seeking out sustainable changes. Prior to the Green Ward Competition, we implemented changed in the way blood tests are sent to patients. Previously, patients would be sent a blood tube in a “Safe lock” box, which had to be sent back to the hospital from a post office, at an inconvenience to the patient. The boxes themselves were expensive and single use, creating a large amount of plastic waste. Use of a lightweight, recyclable plastic pouch with pre-paid postage labels has been implemented, eliminating the trip to the post office (in favour of the closest post box) to the convenience of patients. As clinical nurse specialists we felt uniquely placed to be able to measure the impact across the triple bottom line of sustainable value and promote implementation of this change on a wider scale.
Approach and measurement:
We audited the number of patients suitable for the change to the new blood test kits. The number of the patients in our clinics changes regularly due to starting dialysis or having a transplant. We estimated on average there will be 11 patients under assessment or active on the simultaneous kidney and pancreas register, requiring monthly blood tests, totalling 132 tests annually. On average there will be 30 low clearance (pre-dialysis) clinic patients active on the transplant register who require 3 monthly blood tests, totalling 90 tests annually. This gave as an average annual total of 222 blood tests completed a year.
Environmental: A process-based carbon foot-printing analysis looking at the extraction of the raw materials and disposal was used to estimate the carbon footprint of both kits (blood tests were the same in both kits and therefore excluded from analysis). Data on the type of material was taken from product specification sheets, and each material weighed. It was assumed both kits were disposed of in domestic waste as despite part of the new kit being recyclable, we cannot rely on staff consistently separating and recycling this section. Financial data was used to estimate the carbon emissions associated with postage. For this analysis we looked only at the emissions associated with sending the kits from the hospital to the patient only.
Financial: Postage cost was provided by the hospital postal room.
Social: We conducted semi-structured telephone interviews with previous patients who have used both kits. We also liaised with the Manchester renal transplant coordinators, as their service continues to use Safe Lock boxes, to inspire larger-scale change.
Results:
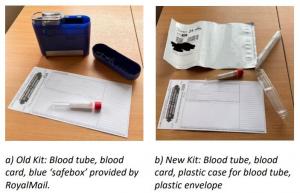
Environmental benefit: The total emissions per test (kit + postage) were reduced by 5.495 kgCO2e, extrapolated across a year with 222 tests sent, this is a saving of 1219.9 kgCO2e. a) Old Kit: Blood tube, blood card, blue ‘safebox’ provided by RoyalMail. b) New Kit: Blood tube, blood card, plastic case for blood tube, plastic envelope
Financial benefit: The old kits cost including postage cost £13.20, whereas the new kits cost £4.41 (3.83 + 58p per plastic container for blood tube). With a saving of £8.79 per kit, we will save £1951.38 per year. With the old kits, we were charged for every kit ordered. With the new kits, we are only charged for blood samples returned, and the envelopes are free, so we won’t be charged for tests that are not completed for patient care.
Social sustainability: Our telephone interviews with patients showed that the new postage kits are easier to use and more convenient to return. Some patients stated they had to pay for the blue lock boxes to be sent a couple of times out of their own money and described them as ‘expensive and seemed unnecessary’. While some patients had no preference for either kit, no negative feedback was received for the new kits.
“I used to use the old lock boxes to send bloods to Manchester. I have to say I really didn’t trust them, they were very bulky but also felt like they wouldn’t close properly so was worried the samples might fall out easily. They weren’t very easy to close.”
“From my house it was 2 miles there 2 miles back so 4 miles in total to post the lock boxes. I also found it quite annoying as I work full time and struggled getting to the post office in time to post them before they closed.”
“I am partially sighted so find it quite fiddly / tricky putting the bloods in here and getting myself to and from the post office.”
For staff, the old lock boxes were described as “fiddly and bulky” so organising and sending out new kits via internal post has been easier and faster for staff in the renal transplant office. Dialysis staff stated they preferred the new smaller postage boxes as the blue boxes were ‘difficult to close properly’.
Clinical and health outcomes: Patient health outcomes have not been negatively impacted by using the new postal kits. Some patients may be able to post their kits more quickly, leading to faster results and care. Some patients have stated rather than driving in a car or using public transport to get their lock boxes to the post office they now walk to their nearest post box instead, which potentially may have indirect benefits of increased physical activity.
Steps taken to ensure lasting change:
Our financial savings have been recognised and celebrated by Paul Jackson, the Abdominal Medicine and Surgery Clinical Service Unit (AMS) project manager for sustainability and transformation and the wider AMS management team. We are also continuing to collaborate with the Manchester renal transplant coordinators. We have shared our data and new postal kit products to support the team in rolling out the same service for their patients. Manchester sends an average of 20 SafeLock blood tests per month. If these 240 tests annually were changed, an additional 1,318.80 kgCO2e and £2,109.60 would be saved. We have regular meetings with other hospitals in the region including Bradford, Hull and York, and plan to present findings here to encourage change to other regional teams. There may be opportunities to share our outcomes further at national network meetings associated with NHS Blood and Transplant or the British Transplant Society to potentially scale our changes to many of the additional 21 transplant centres in the UK.
Leeds Teaching Hospitals NHS Trust - Renal Transplant
Project developed as part of the 2022 Leeds Green Ward Competition. Full impact report available at Green Ward Competition | Centre for Sustainable Healthcare.
Meat-Free Mondays Pledge - Renal Unit

By: Royal Devon and Exeter NHS Foundation Trust
460 kgCO2e (Estimated)
Background: meat, amongst all food, has a high carbon footprint and is more costly than other foods. The renal unit dietician wished to raise awareness amongst staff of the particularly high carbon footprint of meat.
Approach: Kidney Unit staff were invited to sign the ‘Meat-free Monday’ campaign pledge.
Results: 30 staff signed up to the pledge.
Environmental: if staff were not eating a portion of meat once a week this would amount to 598 kgCO2e per year. Eating vegetables instead has approximately 77% of the carbon footprint of meat so the savings would be approximately 460 kgCO2e per year (Carbon factor is 2.5 for meat and 1.73 for vegetarian meals).
Cost: savings to the Trust would depend upon whether the staff were buying food from the hospital or providing their own meals. Vegetarian meals tend to be cheaper than meat-based meals and so there would be a potential saving for the Trust if this measure was adopted at scale in the canteens.
Social: there are potential benefits to staff in joining a movement and in raising awareness of the environmental impacts of our daily choices and habits.
The Centre for Sustainable Healthcare runs the Green Ward Competition as a clinical engagement programme for NHS Trusts wishing to improve their environmental sustainability and reduce their carbon footprint.
Home haemodialysis – Renal Unit

By: Royal Devon and Exeter NHS Foundation Trust
194,700 litres of water/year
£ 1,577
177 kgCO2e
Goal: to assess the value of home haemodialysis compared to in-centre haemodialysis in financial, environmental and social terms. The service currently supports 18 patients to undergo home haemodialysis.
Background: the renal service has been aiming to increase the number of patients receiving haemodialysis at home to improve the financial and environmental impact of haemodialysis as well as to improve the patients’ experience of care. Home haemodialysis uses less water - 152 litres/week/patient on average compared with 360 litres/week/patient in conventional in-centre treatment. Consumables such as plastic and cardboard packaging can be recycled by the local council in the domestic recycling. Utility costs involved in the haemodialysis service are borne by the Trust and reimbursed to the patient. Renal nurses visit the patients at home to oversee care. The process of home haemodialysis is less demanding from a cardiovascular perspective (i.e. less stressful on the heart) as haemodialysis occurs over a longer time. There is evidence that patients undergoing haemodialysis at home:experience an improved symptom profile (improved energy, appetite and sleep), live longer and take fewer medications.
Results: The calculations assume savings as if all these patients were new to the service and would have been on in-centre dialysis. Note that results are based on water use as water use was the largest difference between in-centre and home haemodialysis. Travel (of patients travelling to the units and renal nurses visiting the patients at home) and electricity could also be considered in calculations. A reduction in medication also has a positive impact on the environment, but as there was no data available it has not been included in the calculations.
Cost: savings due to reduced water use amounted to £1,577 per year for the 18 patients.
Environmental: savings of water use per year were 194,688 litres, with a carbon footprint reduction of 177 kgCO2e.
Social/health: there is evidence from the literature of patients undergoing home having a better experience of haemodialysis, however no assessment of the social impact/patient experience was carried out as part of this project.
Renal Unit, RD&E
The project was part of the renal team's efforts in the Green Ward competition run by the Centre for Sustainable Healthcare
Centre for Sustainable Healthcare
Disposing of bicarbonate canisters in general rather than clinical waste – Renal Unit

By: Royal Devon and Exeter NHS Foundation Trust
£498
-280 kgCO2e
: used bicarbonate canisters (Bi-CART) weighing 100g/canister were being put into clinical waste for disposal, which was thought to be an unnecessary expense as disposing of clinical waste is much more costly than disposing of general waste.
Approach: The canisters are now being put in general waste. Results & discussion:
Cost: £498/year in Heavitree unit.
Environmental: The carbon cost of sending the plastic cannisters to landfill increased by 280 kgCO2e/year in the Heavitree unit. Some bicarbonate cannisters (e.g. manufactured by Baxter) can be recycled. Whilst recycling (at a cost of £233.23/tonne) is a more expensive way of processing waste than general waste (at £128.23/tonne), it is cheaper than clinical waste processing (at £350.oo/tonne) and is better from an environmental perspective.
Social: None identified for this project.
Heavitree haemodialysis unit, RD&E
The project was part of the renal team's efforts in the Green Ward competition run by the Centre for Sustainable Healthcare
Centre for Sustainable Healthcare's Green Ward competition
Streamlining disinfection of dialysis machines – Renal Unit

By: Royal Devon and Exeter NHS Foundation Trust
52,416 litres of water/year saved in one dialysis unit.
£1790
4,406 kgCO2e
Background: 24 Gambro dialysis machines are used on the unit. Each day 3 patients use each dialysis machine. After each patient use the machine goes through a heat disinfection cycle to ready it for the next patient (i.e. 3 times/day). In addition, a ‘Hot C-CART’ cycle was run at the end of the day to remove calcium, with a further disinfection cycle overnight.
Approach: The third heat disinfect cycle has been eliminated and the Hot C-CART cycle started following the third patient. This saves 24 heat disinfection cycles saved each day and reduces water and energy use. 11 Results: are given for the savings made at Heavitree. Additional savings would be made if changes were spread to all sites (note that the size of different units varies so the potential for savings would be different at each site).
Cost: £1790/year in Heavitree unit.
Environmental: 4,406 kgCO2e/year at the Heavitree unit. 52,416 litres of water/year in Heavitree unit.
Social: None identified for this project.
Heavitre Dialysis Unit, RD&E
The project was part of the renal team's efforts in the Green Ward competition run by the Centre for Sustainable Healthcare
The Centre for Sustainable Healthcare runs the Green Ward Competition as a clinical engagement programme for NHS Trusts wishing to improve their environmental sustainability and reduce their carbon footprint.
Systematic review of dialysis prescriptions (use of dialysate autoflow facility)

By: Bradford Teaching Hospitals NHS Foundation Trust
£11,524 (Estimated)
3,715kg CO2e (Estimated)
A systematic review of haemodialysis prescriptions was undertaken to optimise and reduce the consumption of water, acid and bicarbonate, by using the dialysate autoflow facility on the Fresenius 5008 machine. Prior to implementation, patients dialysing using the Fresenius 5008 machine used either a 500mls/min or 800 mls/min dialysate flow. Following implementation of this change the options were 500mls/min or autoflow. Autoflow sets the dialysate flow rate to 1.5 times the blood flow rate. Therefore a patient dialysing with a 400mls/min blood flow would have a reduced dialysis fluid flow (600mls/min compared to a previous setting of 800 mls/min). This would allow the use 650g bibags rather than 900g bibags in addition to reduced consumption of water and acid concentrate.
Benefits to the environment
9% reduction in water usage for haemodialysis. 9% reduction in use of acid concentrate, use of smaller Bibags (as above).
The confirmed water saving over the first 8 months has been 95m3 per month, a total of 760m3. Total predicted annual water saving = 1140m3.
Estimated greenhouse gas savings from reduced pharmaceutical procurement (£5,760 saved on bibags + £2,880 saved on acid concentrate, per year = £8,640 total):
= £8,640 x 0.43*
= 3,715 kg CO2e per year
* emissions factor for pharmaceuticals, Annex 13, 2012 Guidelines to Defra / DECC's GHG Conversion Factors for Company Reporting
Cost Benefit to Trust
Investment: staff time only.
Financial savings: direct saving in cost of Bibags of £ 5,760 p.a. plus savings in water and acid concentrates of £2,884 and £ 2,880 respectively = £11,524 per year.
Quality of care: no negative impact on dialysis adequacy.
Details of implementation
The project was implemented by a multi professional team, comprising Gary Carlisle (ward manager), David Croft (chief renal technologist) and Dr John Stoves (consultant nephrologist).
Staff were informed of the planned change and asked to identify patients who would continue to require 900g bibags (i.e. those with 500mls/min blood flow or greater than 4 hours treatment time). Staff were shown how to activate the autoflow facility. Stocks of 650g bibags were increased and a switchover date set. The patients’ dialysis adequacy for the first two months following switchover was compared with dialysis for the two months prior to switchover, to confirm that there was no reduction in the delivered dose of dialysis.
To reduce the environmental and financial and cost of haemodialysis
Joint winner of the 2013 Green Nephrology Award
Reuse of reject water from reverse osmosis for steam production

By: University Hospitals of Bristol NHS Foundation Trust
£15,000 (Estimated)
13,836 kg CO2e / year (Estimated)
Reverse osmosis water purification for dialysis results in large quantities of water being rejected. The rejected water is currently sent to the drains, despite being perfectly clean with a slightly raised mineral content. The project will capture this reject water in the children's dialysis unit at the Bristol Royal Hospital for Children, and direct it to the sump pump at the bottom of the Queen’s building. The pump has previously been used to remove spring water and take it to the boiler house. The reject water will be taken similarly for use in the boiler house to process into steam, saving on mains water demand and reducing water supply and sewerage costs.
Benefits to the environment
Level 8 reverse osmosis plant in the Children’s Hospital currently sends 1m3 of reject water per hour to the drains. There is also 140 litres lost in sanitisation (at least once per week).
Level 6 in the queens building is a smaller plant but will have proportional savings.
Water savings have been calculated for the main Children’s Hospital reverse osmosis plant at 8760m3 per annum. A smaller unit is estimated at half the size: Total annual water savings = 13,140m3 (13.14 million litres).
Estimated greenhouse gas saving = 13,836 kg CO2e / year*
*Conversion factors obtained from the 2012 Guidelines to Defra / DECC's GHG Conversion Factors for Company Reporting (Annex 9, Table 9a): - water supply: 344 kg CO2e / million litres - water treatment: 709 kg CO2e / million litres
Cost Benefit to the Trust
Investment costs: £45,000 for installation of piping and pump
Savings: > £15,000 per year on mains water and sewerage
Anticipated return on investment at 5 years:
= (total saving over 5y – total cost over 5y) / total cost over 5y x 100
= ((£15,000 x 5) - £45,000) / £45,000 x 100
= 67%
Details of implementation
Staff nurse Dan Speakman promoted the idea of RO water reuse through the Trust’s environmental campaign the Big Green Scheme. The initial idea was raised over two years ago. At that stage the focus for invest to save funding was on energy saving projects. Dan has persistently lobbied for the waste water to be captured despite receiving little initial support. His persistence in keeping the idea alive has paid off as water saving has more recently been recognised as an opportunity to make savings. An internal invest to save proposal (consisting of an outline of the project, the estimated costs involved and how savings would be achieved) has now been approved by Trust Finance, and installation is due to complete before the end of 2013.
The installation mainly consists of fitting pipes. A small pump will need to be fitted to get reject water from the smaller plant to join the larger RO reject water it will then be gravity fed to the sump pump that takes spring water up to the boiler house.
Bristol Royal Hospital for Children - Dialysis Unit
To follow example of other kidney units in the Green Nephrology Network, reducing waste of high quality reject water while saving on water and sewerage costs
Green Nephrology network - drew on similar case studies from dialysis units.
Joint winner of the 2013 Green Nephrology Awards: http://sustainablehealthcare.org.uk/green-nephrology/news/2013/09/bradford-and-bristol-royal-share-2013-green-nephrology-award
Received Green Impact award for best environmental idea within University Hospitals Bristol NHS Foundation Trust in 2013.
Doncaster Renal Unit: Paperless Reporting of Routine Dialysis Haematology and Biochemistry Results
By: Doncaster and Bassetlaw Hospitals NHS Foundation Trust
Freeing up administrative and clinical time and reducing the size and weight of notes (with resulting reduction in the costs of transport and storage and improvements in readability of the notes files). Reduction in unnecessary paper reports should reduce the risk of important results being lost, with consequent benefits to patient safety. A recent adverse incident where a microbiology report was not seen was probably in part caused by the excessive amount of unnecessary reports.
£120 (Estimated)
380kg CO2 (Estimated)
Routine monthly haemodialysis blood tests generate a very large amount of paper results (at least 20000 sheets of A4 paper per year for the approximately 160 patients on the DBH dialysis program). Such large volumes of paper result in significant clinical and administrative workload and a high risk of relevant reports being missed. All such results are reviewed electronically in the monthly dialysis MDT meetings. Given the costs and lack of utility of paper reports it was agreed with the Trust's medical director that paper reports for routine haemodialysis results could be switched off.
Details of implementationThe first step was to agree with the Trust's medical director that not having paper results did not create a risk to patient safety or a medico-legal problem. Once this had been agreed, the Medical Records department were informed to ensure that a record is kept of which notes are affected and what results are not being filed on paper.
The pathology IT manager assigned location codes to each dialysis unit and, in March 2012, set the pathology system to paperless reporting of haematology and biochemistry reports for these locations. Staff in the haemodialysis units and pathology specimen reception were informed of the relevant codes to ensure samples are booked in correctly.
Benefits to environmental sustainabilityThe annual costs of printing 20,000 sheets of A4 paper (calculated using Hewlett-Packard's online tool) are:
- Energy 563 kWh
- Paper: 100kg
- Energy & paper CO2 emissions: 380kg CO2
- Energy & paper costs: £120
Doncaster Royal Infirmary
To reduce paperwork and filing backlogs, to free up clinical and administrative time, to reduce the risk of important results (eg microbiology reports) being missed and to reduce costs associated with printing.
Remote CKD monitoring as part of a Disease Management Program
By: Sheffield Teaching Hospitals NHS Foundation Trust
These are still early days but generally patients and staff have responded very positively as people can receive care closer to home without losing touch with secondary care.
CKD management is predominantly data-driven. Considerable IT infrastructure is already in place that has enabled a remote CKD monitoring service for patients in Sheffield enabling devolved, patient centred care. A future renal database is likely to be able to increase the sophistication of such a disease management program. The start-up costs for such a model mainly consist of a salary for one clinical nurse specialist with modest consultant nephrologist support.
Current model of CKD care in Sheffield
The Sheffield Kidney Institute (SKI) in collaboration with primary care has introduced a number of measures to improve the recognition and management of chronic kidney disease (CKD) in the community whilst ensuring referrals to secondary care are ‘managed’ in an appropriate way.
These include:
- Online guidelines covering both the referral and management of CKD in primary care.
- Online educational package covering the management of CKD in primary care.
- Allocation of 1 PA of consultant time to screen referrals and advise GPs about which patients can be managed in primary care with appropriate management plans. Since the start of this service in 2006 approximately 30% of referrals from primary care have been dealt with through advice and guidance thereby avoiding unnecessary trips to secondary care. This service meets a key UK Renal Association standard that renal units should provide a non-visit based advisory service for primary care.
- In addition to the paper-based system above secure, electronic, consultant lead advice and guidance is available to primary through both the Choose and Book system as well through email via an nhs.net account.
Further to these measures, the SKI has identified a group of patients with CKD who currently remain under specialist kidney care but who could be effectively managed in primary care, with specialist support. These are patients with stable/slowly progressive but advanced CKD, who require regular biochemical and blood pressure monitoring, or who require specialist anaemia management.
The problem
Although the number of patients discharged to primary care has increased significantly, discharge rates from secondary care may be limited by concerns about whether patients can be reliably locked into a disease management programme in primary care. Indeed there is data to support such concern. For example the variability in prevalence of CKD by practice within Sheffield PCT ranges between 0% and 9.8%. Whilst some of this variation undoubtedly reflects practice-population demographics it is likely that systems for identifying and monitoring CKD varies between practices. Similarly, only 65% of patients in Sheffield PCT achieved the combined QOF indicators of being on a CKD register and attaining target blood pressure.
Proposed model of care
We aim to develop the renal database (Proton) at the Sheffield Kidney Institute (SKI) to allow remote monitoring of patients with CKD. This is being done at the moment with the Sheffield Central Consortium of GP practices.
The key changes we have implemented are:
- Clinician-led CKD-Disease Management Program (CKD-DMP) specifying frequency of laboratory and blood pressure testing with individualised targets for care.
- All patients suitable for CKD-DMP to have bloods taken in primary care and self-monitor blood pressure or have blood pressure taken in GP surgeries
- To utilise a CKD nurse specialist to manage the remote data, liaise with patient and primary care physicians to replace clinic visits with a tele-consultation, reviewing clinical data with patient whilst maintaining care as set out by treatment targets in CKD-DMP.
Which personnel were involved?
CKD specialist nurse and consultant nephrologist in secondary care. Practice nurse in each surgery who acts as CKD link for specialist nurse
What was the timeframe?
Pilot started within 6 months of agreement between primary and secondary care.
Has the initiative been implemented elsewhere, before or since?
Not to our knowledge, though Bradford does have a well developed e-consultation service. This is different, being a remote monitoring and management service for chronic disease.
Sustainability benefits
The introduction of remote monitoring with tele-consultation has the potential to improve the targeting of specialist care resources (financial and environmental) to deliver the maximum value to patients. By involving patients in self-monitoring, the model could potentially enhance patient empowerment in the management of their care, while reducing the need for travel as services are provided closer to home.
No capital costs were required as the lab data already uploads data onto the renal database. Resource required in terms of specialist nurse time, consultant time and practice nurse/GP time
