- Group home
- You must register/login in order to post into this group.
Changing the 3 monthly blood test postage kits for patients on the renal transplant register
By: Leeds Teaching Hospitals NHS Trust
Please see social sustainability and clinical and health outcomes sections below
£1951.38 (Actual)
1219.9 kgCO2e (Actual)
Team members:
- Natalie Bird - Clinical Nurse Specialist, Renal Transplant
- Laura Kirk - Clinical Nurse Specialist, Renal Transplant
- Jo Wales - Clinical Nurse Specialist, Live Renal Donation
- Jo Hitchings - Senior Clinical Support Worker
Project aims:
To measure the environmental, social and financial benefits of a new postal system compared with an old postal system.
Background:
Patients active on the transplant register and those listed for simultaneous kidney and pancreas transplant must have regular blood tests (every 1-3 months) to re-examine their antibodies. With patients all over the region, transporting these samples to the laboratory can be logistically challenging and expensive.
As a team, the renal transplant department is already very proactive in seeking out sustainable changes. Prior to the Green Ward Competition, we implemented changed in the way blood tests are sent to patients. Previously, patients would be sent a blood tube in a “Safe lock” box, which had to be sent back to the hospital from a post office, at an inconvenience to the patient. The boxes themselves were expensive and single use, creating a large amount of plastic waste. Use of a lightweight, recyclable plastic pouch with pre-paid postage labels has been implemented, eliminating the trip to the post office (in favour of the closest post box) to the convenience of patients. As clinical nurse specialists we felt uniquely placed to be able to measure the impact across the triple bottom line of sustainable value and promote implementation of this change on a wider scale.
Approach and measurement:
We audited the number of patients suitable for the change to the new blood test kits. The number of the patients in our clinics changes regularly due to starting dialysis or having a transplant. We estimated on average there will be 11 patients under assessment or active on the simultaneous kidney and pancreas register, requiring monthly blood tests, totalling 132 tests annually. On average there will be 30 low clearance (pre-dialysis) clinic patients active on the transplant register who require 3 monthly blood tests, totalling 90 tests annually. This gave as an average annual total of 222 blood tests completed a year.
Environmental: A process-based carbon foot-printing analysis looking at the extraction of the raw materials and disposal was used to estimate the carbon footprint of both kits (blood tests were the same in both kits and therefore excluded from analysis). Data on the type of material was taken from product specification sheets, and each material weighed. It was assumed both kits were disposed of in domestic waste as despite part of the new kit being recyclable, we cannot rely on staff consistently separating and recycling this section. Financial data was used to estimate the carbon emissions associated with postage. For this analysis we looked only at the emissions associated with sending the kits from the hospital to the patient only.
Financial: Postage cost was provided by the hospital postal room.
Social: We conducted semi-structured telephone interviews with previous patients who have used both kits. We also liaised with the Manchester renal transplant coordinators, as their service continues to use Safe Lock boxes, to inspire larger-scale change.
Results:
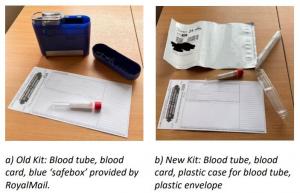
Environmental benefit: The total emissions per test (kit + postage) were reduced by 5.495 kgCO2e, extrapolated across a year with 222 tests sent, this is a saving of 1219.9 kgCO2e. a) Old Kit: Blood tube, blood card, blue ‘safebox’ provided by RoyalMail. b) New Kit: Blood tube, blood card, plastic case for blood tube, plastic envelope
Financial benefit: The old kits cost including postage cost £13.20, whereas the new kits cost £4.41 (3.83 + 58p per plastic container for blood tube). With a saving of £8.79 per kit, we will save £1951.38 per year. With the old kits, we were charged for every kit ordered. With the new kits, we are only charged for blood samples returned, and the envelopes are free, so we won’t be charged for tests that are not completed for patient care.
Social sustainability: Our telephone interviews with patients showed that the new postage kits are easier to use and more convenient to return. Some patients stated they had to pay for the blue lock boxes to be sent a couple of times out of their own money and described them as ‘expensive and seemed unnecessary’. While some patients had no preference for either kit, no negative feedback was received for the new kits.
“I used to use the old lock boxes to send bloods to Manchester. I have to say I really didn’t trust them, they were very bulky but also felt like they wouldn’t close properly so was worried the samples might fall out easily. They weren’t very easy to close.”
“From my house it was 2 miles there 2 miles back so 4 miles in total to post the lock boxes. I also found it quite annoying as I work full time and struggled getting to the post office in time to post them before they closed.”
“I am partially sighted so find it quite fiddly / tricky putting the bloods in here and getting myself to and from the post office.”
For staff, the old lock boxes were described as “fiddly and bulky” so organising and sending out new kits via internal post has been easier and faster for staff in the renal transplant office. Dialysis staff stated they preferred the new smaller postage boxes as the blue boxes were ‘difficult to close properly’.
Clinical and health outcomes: Patient health outcomes have not been negatively impacted by using the new postal kits. Some patients may be able to post their kits more quickly, leading to faster results and care. Some patients have stated rather than driving in a car or using public transport to get their lock boxes to the post office they now walk to their nearest post box instead, which potentially may have indirect benefits of increased physical activity.
Steps taken to ensure lasting change:
Our financial savings have been recognised and celebrated by Paul Jackson, the Abdominal Medicine and Surgery Clinical Service Unit (AMS) project manager for sustainability and transformation and the wider AMS management team. We are also continuing to collaborate with the Manchester renal transplant coordinators. We have shared our data and new postal kit products to support the team in rolling out the same service for their patients. Manchester sends an average of 20 SafeLock blood tests per month. If these 240 tests annually were changed, an additional 1,318.80 kgCO2e and £2,109.60 would be saved. We have regular meetings with other hospitals in the region including Bradford, Hull and York, and plan to present findings here to encourage change to other regional teams. There may be opportunities to share our outcomes further at national network meetings associated with NHS Blood and Transplant or the British Transplant Society to potentially scale our changes to many of the additional 21 transplant centres in the UK.
Leeds Teaching Hospitals NHS Trust - Renal Transplant
Project developed as part of the 2022 Leeds Green Ward Competition. Full impact report available at Green Ward Competition | Centre for Sustainable Healthcare.
