Green nephrology
Reducing Waste in the Dialysis Unit Queen Margaret Hospital, Dunfermline

By: NHS Fife
Reduced clinical waste, 21.5 tonnes per year
£14907.10 (Actual)
26.847 tonnes CO2e / year (Estimated)
The dialysis unit at the Queen Margaret Hospital, Dunfermline, has 20 stations and provides over 13,000 treatments per year. Mary Thompson, a dialysis nurse in unit, ran a series of Waste Watch Weeks there in 2009, and identified opportunities to improve practice.
The unit has recently moved towards providing online haemodiafiltration (HDF) using 15 Fresenius 5008 machines. Mary noted that, for every dialysis session, a one litre bag of normal saline was used to re-infuse the patient’s blood at the end of the treatment. This bag would be opened and attached to a giving set at the start of the treatment (ready for use should the patient suffer a hypotensive episode during their dialysis treatment), despite the fact that the newer haemodiafiltration machines were able to prepare ultrapure sterile substitution fluid directly from the dialysate by directing it through an ultrafilter.
When it came to re-infusing the patients blood at the end of the treatment, only 200 mls of this fluid would typically be required. The remaining 800mls of normal saline, the plastic bag containing it, and the plastic giving set were then all placed in an orange bag – along with the extracorporeal circuit and bicarbonate bag - and disposed of through the clinical waste stream. Mary realised that there were a number of opportunities to reduce…
REDUCTION 1
The use of saline and giving sets was reduced by stopping the unnecessary practice of hanging a bag for emergencies in favour of using the online facilities for emergencies and re-infusion. This saved not only the carbon embodied in their manufacture, but also the emissions associated with their disposal.
A bag of normal saline was costing the dialysis unit £0.52, whilst a single giving set was costing £0.35. During the course of the 10,764 treatments provided per year, the use of online substitution fluid saves £9,364 (minus the small but less quantifiable cost of producing the exact fluid volumes online) in procurement costs alone (waste disposal savings are outlined below).
REDUCTION 2
The amount of clinical waste was further reduced by improving segregation at source. The first measure had already removed a partially filled bag of normal saline and giving set from the waste stream, but the bicarbonate bag could also be diverted away from the clinical waste stream to domestic waste.
Bicarbonate is added to the dialysate throughout the treatment. Although it is sometimes supplied in plastic containers (see the Recycling Case Study), in Mary’s unit the bicarbonate is provided in bags (often referred to as B-Bags). Mary realised that these bags could be placed in the domestic waste stream after each treatment (as ongoing efforts to find a facility willing to recycle them have proven unsuccessful).
These two initiatives had reduced the clinical waste from a single treatment by 2 kg through the removal of one bag of reperfusion saline (usually with 800 mls remaining in it), one giving set and the bicarbonate bag. Over the annual 10,764 treatments provided by the unit using Fresenius 5008 machines, this would result in a reduction in clinical waste of 21,528 kg – or 21.5 tonnes. As a relatively large producer of clinical waste, the Queen Mary Hospital was charged at £300 per tonne of clinical waste, leading to an annual saving of £6458.40. This saving was offset by the increased cost of the domestic waste (£85 per tonne) attributable to the addition of the bicarbonate bag to this waste stream. The annual 10,764 treatments produce 10,764 bicarbonate bags, with a total weight of 10.764 tonnes and a disposal cost of £914.90, resulting in an overall annual saving of £5543.10.
Quantifying carbon savings (section added October 2012)
Greenhouse gas (GHG) conversion factors for procurement of pharmaceuticals and medical equipment were obtained from the 2012 Guidelines to Defra / DECC's GHG Conversion Factors for Company Reporting (Table 13). Using these factors we estimated the GHG savings per year from avoided procurement of saline bags and giving sets:
- Reduction in pharmaceutical procurement (saline bags): £0.52 x 10764 treatments = £5597.28 / year. £5597.28 x 0.43 kg CO2e/£ = 2.407 tonnes CO2e
- Reduction in medical equipment procurement (giving sets): £0.35 x 10764 treatments = £3767.40 / year. £3767.40 x 0.30 kg CO2e/£ = 1.130 tonnes CO2e
Greenhouse gas (GHG) conversion factors for waste disposal were obtained from the 2011 Guidelines to Defra / DECC's GHG Conversion Factors for Company Reporting (Table 9d). The GHG for incineration of clinical waste was taken as 1,833 kg CO2e emitted per tonne of waste (DEFRA emissions factors for incineration do not specifically account for clinical waste, which is commonly undertaken at higher temperatures. To reflect the increased emissions that are likely to result from the incineration of clinical waste, the highest available emissions factor for incineration was applied). The GHG for landfill of plastic waste was taken as 34 kg CO2e per tonne.
- Previous GHG emissions from disposing saline bags + giving sets + bibags as clinical waste, per year:Saline bag + giving set + bibag - 800ml residual saline = 1.2kg1.2kg x 10764 treatments = 12.917 tonnes. 12.917 tonnes x 1833 kg CO2e/tonne = 23.676 tonnes CO2e / year
- Current GHG from disposing bibags (1kg) as domestic waste, per year:1kg x 10764 treatments = 10.764 tonnes / year. 10.764 tonnes x 34 kg CO2e/tonne = 0.366 tonnes CO2e / year
- Net savings from waste disposal = 23.676 - 0.366 = 23.310 tonnes CO2e / year
Combined GHG savings (procurement and waste) = 1.130 + 2.407 + 23.310 = 26.847 tonnes CO2e / year
Queen Margaret Hospital, Whitefield Road, Dunfermline, Fife, KY12 0SU
To reduce waste and its associated disposal costs
Telephone Clinics in Follow-Up of Renal Transplant Recipients - Case Study and How to Guide

By: University Hospitals Coventry and Warwickshire NHS Trust
heightened sense of empowerment in the management of the patients' medical problems, more convenient access to healthcare and considerable time savings for patients
2000kg CO2 The carbon savings of telephone clinics will of course vary between different renal units catering for different geographical areas and patient numbers. A ball-park figure for the carbon savings attributable to replacing a single face-to-face clinic with telephone consultations can be made by undertaking a simple transport survey on patients attending clinic. (Estimated)
The renal unit at the University Hospital of Coventry and Warwickshire has been successfully running a twice-monthly telephone clinic to provide follow up to transplant patients since 2006 to reduce the inconvenience to patients of frequent trips to hospital. Telephone clinics are offered to patients at the discretion of the clinical team. Patients must have a stable transplant function, and factors such as the patient's hearing and co-morbidities are also considered. Patients who are suitable for telephone follow-ups are offered the choice to remain in the traditional follow up system or switch to quarterly telephone clinic follow up, with just one annual traditional (‘face-to-face’) outpatient appointment at their local renal clinic.
The UCHW service now provides follow up to approximately 125 of the 360 patients with stable transplants of more than one year's standing.
In preparation for a telephone consultation, patients undertake their blood tests in the normal way (at UHCW this entails visiting either their GP, one of four local hospitals, or the city centre phlebotomist service). Patients are also asked to provide up-to-date blood pressure and weight readings (which can either be taken at home or at the Family Practice). Telephone appointments are scheduled to last 10-15 minutes, and the patients ring in at designated times. Letters are sent to GP’s in the normal manner. Blood test forms are sent out to patients along with their next appointment time.
Patient Safety Risk Management
Patients in whom follow-up is predominantly telephone-based may be examined by clinicians less frequently and this may introduce a risk to patient safety. Although further research is undoubtedly required, the medical literature does not appear to indicate that telephone consultations increase the risk to patient safety when used to provide routine follow up of patients with chronic diseases. Indeed, some studies show the opposite effect. However, efforts should be made to reduce the risk to patient safety in all aspects of clinical care, and two clear measures exist in relation to telephone consultations. Firstly, the exclusion of patients for whom telephone consultations might be inappropriate is vital. Secondly, should a clinician undertaking a telephone consultation identify a need to examine a patient, the system must allow the organisation of a face-to-face review in a timely and convenient fashion. The possibility of missing skin cancers may be a particular concern to clinicians providing telephone-based care for renal transplant recipients taking immunosuppressants. All patients, irrespective of their follow up modality, should be educated to look for and report new or changing skin lesions. In reality, those patients with a prior history of skin cancer will have open access to the local dermatology service. Those reporting their first skin lesion will usually be seen faster if referred by their General Practitioner (under the ‘2 week wait’ referral system for suspected skin cancers). The practice of the clinicians in the University Hospital of Coventry and Warwickshire telephone unit is therefore to ask these patients to seek a review (and possible referral) by their General Practitioner.
GETTING STARTED – ‘HOW TO’ GUIDE
Ascertain the size and frequency of the telephone clinic you wish to run.
1. Determine the catchment population for the telephone clinic. You may wish, eventually, to offer the service to all renal transplant patients under the care of the renal service. However, it may be simpler to begin by running a telephone clinic to cater for those patients under the care of a particular consultant.
2. Within this catchment population, estimate the potential number of patients that might be suitable for follow up by telephone clinic. Start by identifying the number of patients with stable renal transplants of more than one year’s standing. You might choose to ask these patients, at this early stage, whether they would be likely to opt for telephone consultations. This would provide you with a good understanding of the capacity to which to develop the transplant clinic. It would also allow you to return to these patients directly once the opportunity to book patients into the clinic arises, hopefully reducing the period for which the clinic is ‘underfilled’.
3. Clarify how many patients you envisage enrolling in the transplant clinic. Perhaps begin slowly, by developing a clinic with capacity to follow up around 10-20% of the patients with stable renal transplants (as, of course, not every one of the patients you have identified so far will meet the necessary criteria, or indeed wish to switch to follow up by telephone) or around 50% of those patients who have indicated that they would prefer to be followed up in this way.
4. Given the number of patients you intend to follow up by telephone consultation, the approximate frequency with which you plan to review them, and the duration of time you anticipate allocating to each consultation (usually 10-15 minutes), ascertain how frequently you will need to hold telephone clinics.
Consider the resources you will require.
5. Ensure that your department will have the necessary resources and administrative support to run the clinic. Once the telephone clinic is running near to its intended full capacity, the reduction in the number of consultations in other clinics should ‘free up’ the staff and resources required for the telephone clinic, but this might not happen immediately.
6. Identify where you will run the clinic. For example, by moving the clinic to your office you will free up a room in the outpatient department (but you would need to re-organise the delivery of patient notes).
7. Identify how patient blood tests will be undertaken. Any departure from current practice may have costing implications. Also, where necessary also consider how results will be retrieved, and whose responsibility this will be.
Determine how your unit will be funded for the telephone clinic.
8. Involve the Contracting Department in your hospital in order to commence negotiations with the Primary Care Trust commissioning body.
9. Ensure that any agreed tariff fully covers the activities entailed in the running of the telephone clinic.
Further tips
1. Ensure that patients appreciate that they can return to face-to-face appointments at a later date if they choose to do so.
2. It is important that the Trust and commissioning body define the unit of care covered by any agreed tariff. For example, it might be important to state whether or not impromptu phone calls between patients and clinicians that occur between designated telephone clinic appointments will also count as consultations.
University Hospital of Coventry and Warwickshire
To reduce the inconvenience to patients of frequent trips to hospitals
Financial Security The likely discrepancy between the suggested PbR tariff for non-face-to-face activity (£23) and the re-imbursement that a Trust currently receives for providing its existing outpatient clinic service means that there is a potential financial risk to the Trust whereby the tariff does not cover the full cost of running a telephone clinic. This risk is avoidable as the tariff for non-face-to-face activity is negotiable and must be agreed in advance with the commissioning body, allowing Trusts the opportunity not to introduce the service where tariffs might be insufficient. As, in most cases, the telephone clinic will simply replace the existing face-to-face activity, we would suggest that Trusts are well placed to argue that it should be financially supported.
Conserving Water in Haemodialysis - Case Study and How To Guide
By: East Kent Hospitals University NHS Foundation Trust
Considerable savings on mains water and sewerage costs, good for the environment as water is a finite natural resource, compliance with carbon targets
£7,500 (Actual)
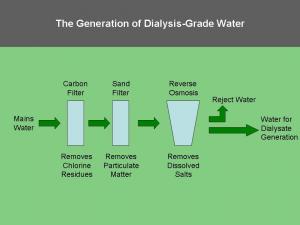
Haemodialysis consumes vast quantities of water. Producing the 120 litres of dialysate required for a typical four hour session requires approximately 400 litres of mains water. Reverse osmosis is an important step in the purification process for water used in haemodialysis. Reverse osmosis systems reject up to two thirds of the water presented to them. This 'reject water' does not come into contact with the patient at any stage and poses no infection risk, yet it is 'lost to drain' in almost all dialysis facilities.
In 1999, two years after the Canterbury dialysis unit installed a new reverse osmosis plant, a simple system capable of recycling 800 litres of reject water per hour was installed at a cost of £15,000 with the help of the hospitals estate department. The system has now been running for over 10 years, saving the Trust £7,500 per year on mains water and sewerage costs.
The salvaged reject water is directed to a recovery tank in the basement. From there it is pumped up to the grey water tank on the roof, which then supplies the water to the hospital toilets. Float switches divert reject water to the drain if the grey water tank is full, and diverter valves direct the reject water directly to the drain from the reverse osmosis system during monthly chemical desinfections.
Investment Appraisal
The return on investment will depend upon:
1. The investment: the cost of installation & maintenance.
2. The return: the savings on mains water and waste water. This can be calculated by multiplying the regional mains water and waste water rates by the volume of reject water which the system is able to provide in place of mains water for an alternative use (e.g. laundry). It is useful to factor in projected price rises and changes in demand to gain a view of future potential savings.
Risk Management
Careful planning and calculations will prevent the implementation of a project which is financially inviable due to physical barriers or miscalculations regarding the amount of reject water produced.
The new use supplied by the recycled water needs a back-up mains supply.
Calculation of Carbon Savings
Carbon savings (kg CO2e/year)
=
[Volume water saved in one year (L) x mains water carbon conversion factor (kgCO2e/L)], e.g. DEFRA
-
[electricity used for pumping per year (kWh) x carbon conversion factor (kgCO2e/KWh)]
How To Guide - Getting started:
1. Discuss the idea with your Renal Technician. They will play a vital role in any water conservation project, understanding the local set-up better than anyone else.
2. Involve your local Estates department. The support and advice of the hospital Estates department is also vital. Their engagement may require the presentation of a sound business case. In most cases, it will be the Estates department that benefit financially from the methodology.
3. Clarify the scenario. Will the methodology be implemented into the design of a ‘new build’ dialysis unit, at the time of replacing the RO system in an existing dialysis unit, or perhaps alongside an existing and satisfactory RO system already in place in a dialysis unit? These different scenarios will influence the total costs involved, but the return on investment may still make the project worthwhile.
4. Clarify the potential volume of reject water that will be salvaged each year.
In order to maximise the financial and environmental benefits of the project, it is important to match the volume of reject water available to an alternative use that requires a similar volume. Many reverse osmosis systems record the volume of reject water produced, but this can be ascertained with a simple flow meter if necessary. It should be remembered that, where reverse osmosis systems are being replaced, the newer system is likely to be more efficient and produce less reject water.
5. Assess the quality of the reject water to be salvaged. The precise quality of the reject water produced will vary from region to region. Whilst it will almost always meet the requirements for its intended use, it is vital that this is assured prior to proceeding further. Your renal technician will be well versed in checking the water quality.
6. Given the volume and quality of the reject water available, now identify the intended use for this water. Possibilities include: sanitation, laundry, boiler feed, sterilisation units and irrigation – on site or supplied to a neighbouring facility. Practical considerations are important. For example, salvaged reject water can only be used in laundry services if the plumbing required is feasible and affordable.
7. Calculate the financial cost per year of the current practice of supplying mains water for this intended use. This will require knowledge of the mains water rates for your hospital, information which the Estates department can provide.
8. Calculate the financial savings resulting from the reduction in waste water from the haemodialysis unit. This will require knowledge of the waste-water rates for your hospital. Remember that some reject water may still be lost to drain if it exceeds the demand/capacity of the salvage system, and during disinfection cycles.
9. Calculate the initial total financial expenditure incurred in implementing the methodology (including the infrastructure required to transport the reject water to the place of use). Costs may include: storage tanks, pipework, pumps and installation costs. Maintenance costs are likely to be small.
10. From these figures, develop a repayment projection and calculate the breakeven point (the point in time by which the savings - due to reduced mains water and reduced losses-to-drain - might be anticipated to have recouped the investment costs of the methodology, and from whence the use of reject water for the new purpose realises potential savings).
11. Convince your Trust to fund the work. Whilst this will certainly require the support of your Estates department, it may also require the approval of the Director of Finance. It is also worth applying for funding from Salix Finance, an organisation set up by the Carbon Trust to deliver interest free funding to accelerate investment in energy efficiency technologies within the UK public sector. Their website is http://www.salixfinance.co.uk/home.html
12. System maintenance should become part of routine estates plant room inspections - a simple check function tick list is sufficient. Water storage tanks will require cleaning in line with Trust protocols for other tanks in the hospital.
Canterbury dialysis unit and satellite dialysis unit in Ashford
Large volumes of 'reject' water were lost to the drains
Hospital's estate department
- « first
- ‹ previous
- 1
- 2
- 3
- 4
