Green nephrology
Pilot Study of a Kidney Patient Results Monitoring Service
By: Royal Cornwall Hospitals NHS Trust
95% patients were happy with the way they received results. 86% patients felt that having blood tests taken at the surgery saved them time, money and the stress of travelling to hospital
£12,160 (Actual)
760kg CO2e (Estimated)
The renal department at the Royal Cornwall Hospitals NHS Trust conducted a ten month pilot study of a Kidney Patient Results Review Monitoring Service from June 2011 to March 2012. Patients with chronic kidney disease (CKD) III and IV were managed in primary care with secondary care supervision of blood results. Funding was offered via the Southwest Peninsula Network to set up a ‘virtual’ CKD clinic. Our team took up this opportunity, recognising the particular benefits in Cornwall, where rural patients currently travel long distances. The lead consultant was Dr. Rob Parry, supported by PRMS nurse, Mel Geall.The model successfully reduced the number of patient visits to renal outpatients, saving on patient time and travel, without compromising care.
Benefits to environmental sustainability
During the pilot, a total of 135 patients came under the review service, 119 of them were reviewed, with 95 clinic visits being saved. Mileage between the patients’ homes and the hospital where they attended their renal outpatient clinic were calculated using the ‘RAC Routeplanner’ website. A total of 2,020 miles were ‘saved’ resulting in a saving of 2020 miles x 0.37604 kgCO2e per mile* = 760 kgCO2e
It is also worth noting that some patients would be travelling to their appointments by ambulance or hospital funded transport.Two patients, who live on the Isles of Scilly, used to be flown by helicopter for each visit.
* total GHG conversion factor for medium cars using unknown fuel, taken from Annex 6 (Passenger Transport) of Defra 2012 greenhouse gas conversion factors for company reporting, available from: http://www.defra.gov.uk/publications/2012/05/30/pb13773-2012-ghg-conversion/)
Cost benefit
Costs: The pilot had funding for 1 day/week Band 6 specialist nurse and 2 hours/week consultant time (approx. £10,000 in total).
Savings: 175 tests were reviewed remotely, saving 95 clinic visits at a tariff of £128* = £12,160.
* 2011-12 PbR tariff for follow up attendance in nephrology, single professional
To see if carbon and patient time and money could be saved without compromising care
Negotiation is currently under way to agree a tariff to non face-to-face review, which will allow the service to continue long term.
Logistically, looking at all patients blood resultsis relatively straight forward, but monitoring patients bloods alone does not fulfil the requirements of the Renal National Service Framework. GPs are now being asked to ensure PRMS patients have blood pressure checked and urinalysis carried out.
Patient numbers in the survey have been limited due to the limited time frame of study.
Reverse Osmosis Waste Water Recycling

By: Countess of Chester Hospital NHS Foundation Trust
Water saving: 1,460,000 litres / year
£3,144 (Estimated)
116.48kg CO2e (Estimated)
The Chester Green Nephrology Local Representative has led the development of a business case to enable the haemodialysis unit to recycle its 'grey' reject water produced by the reverse osmosis plant, which provides the purified water for dialysate. The plant runs for 123 hours per week, producing between 8.7-14.2 litres litres waste water per minute, just under a quarter of the annual water consumption within the Trust. If the project is implemented, the water will be stored and used for a regeneration of the carbon filters within the treatment plant, number of toilets, a sluice area, and a laundry area located in the renal outpatients department.
The project has been inspired by a previous Green Nephrology case study which was presented at the British Renal Society conference in 2010. Following this, the Chester Green Nephrology Local Representative, Elizabeth Critchley, proposed the introduction of waste water recycling to the carbon reduction team in Chester, who showed a keen interest. The calculations for water savings have been made in conjunction with a local water company, which has also given a a quote for the works.
Other people who have been approached within the Trust include the Renal Unit Manager, the EBME manager (responsible for RO plant maintenance), and the Estates department. The business case has now been submitted to the Trust carbon reduction team, who are supportive and will present it to the Board.
The water company undertaking the future works will be responsible for fitting the water tank, piping and connections to the plant room, roof space, toilets, sluice and laundry area. This work will be performed overnight and on Sundays when the plant is not being used, to eliminate any risk to the water pressures during operational times as this could pose unnecessary risk to patients on dialysis.
Benefits to environmental sustainability
The forecasted water saving is 4,000 litres per day 1,460 cubic metres per annum. Daily saving usage:
- Water Reused by Carbon Filters - 1 backwash/day = 900 litres/day
- Water Reused by Softeners - 2 regenerations/3 days = 500 litres/day
- Available water for washing machines and toilet flushing = 2,600 litres/day
This amount equates to an approximate reduction in carbon emissions of 0.11648 tonnes CO2e per annum*.
Conversion factors used:
Water supply: 0.39 kgCO2/m3 - figure supplied by Welsh Water the Trust current water supplier
Sewerage: 0.17 kgCO2/m3 - figure supplied by the Environmental Agency
Financial benefits
The Trust will also make a financial saving of
- Tap Water: £1370.79 per annum (£0.9389 per m3 of water)
- Sewerage Services: £1773.17 per annum (£1.2145 per m3)
- Total Annual saving = £3143.96
The Trust will be making a financial investment of £11,030, therefore the retrofit will have paid for itself within 3 years 6 months.
Wychwood Water Systems Ltd
Lighting Project

By: Bradford Teaching Hospitals NHS Foundation Trust
Additional benefits include an improvement in measured lighting levels and reduced maintenance costs as the new light fittings have a longer life span. An informal post-evaluation survey has shown that staff are happier with the increased levels of lighting. Apart from an improved working environment the project contributes to the achievement of the Trust's sustainable development goals and a redution in its climate change levy.
£612 per year (Estimated)
2.3 tonnes CO2e per year (Estimated)
The renal service decided to invest the full value of a BJRM Innovation in Renal Medicine Award 2011 prize (£5,000) in a greener healthcare energy saving initiative. Following a site survey of the renal unit, the lighting project was chosen as the most appealing in terms of delivery, risk and savings. The survey revealed that the fluorescent light fittings were of a 'T8' type, whose energy consumption can be up to two times that of a modern 'T5' light fitting. Existing luminaires had started to degrade and could not produce all the expected light from the fluorescent tubes. Following a consultation exercise with renal unit staff, a plan was agreed to install 'T5' light fittings. A total of 85 light fittings were changed in the Renal unit offices and wards.
The project was part of an on-going collaboration between the local Green Nephrology Champion and the Trust Estates department. The feasibility study, survey and business case were carried out by Mr Nsipa Siwale (Energy Manager). Activities included risk assessments, product selection, tendering and project management. Departmental support and funding was provided by Dr John Stoves. To minimise risks and disruption to staff and patients, most of the work was carried out after normal working hours.
Benefits to environmental sustainability
The annual operating hours for lighting in the Renal unit are 3,000 hours. The average energy saving per individual light is 36 kilowatt hours per year. Based on a greenhouse gas conversion factor of 0.58982 kgCO2e/kWh*, the project will save 11.5 tonnes of CO2e over 5 years.
* “All-scopes grid rolling average” emissions factor for electricity consumed (2010), Table 3c, Defra 2012 greenhouse gas conversion factors for company reporting
The main aim of the project was to reduce carbon emissions. The consultation exercise also revealed the need to improve levels of illumination in the unit, for example in the rooms used by technical staff.
The contractor for the project was JA Richardson Ltd, an experienced contractor who has undertaken several jobs successfully at the Trust with an excellent knowledge of the Trust and good Health and safety track record in the execution of similar projects.
A solar panel installation project may contribute to a further reduction in future charges.
Retrofit of Heat Exchangers to Dialysis Machines
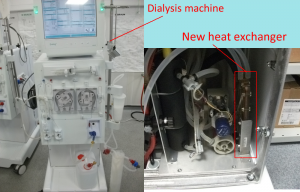
By: Newcastle Upon Tyne Hospitals NHS Foundation Trust
Reduced electricity bills for home dialysis patients
£327.60 - but likely to increase in Winter (Estimated)
1.207 tonnes - but likely to increase in Winter (Estimated)
Heat exchangers have been retrofitted to all 21 BBraun Dialog+ Dialysis Machines for patients on home haemodialysis. The decision was taken to prioritise retrofit of home haemodialysis machines after analysis of temperature changes and power consumption in the home and dialysis unit settings. The colder incoming water in patients' homes in Winter, as compared with the water temperature in the dialysis centre, resulted in increased power consumption over all and greater energysavings from inclusion of the heat exchanger.
Benefits to environmental sustainability
Estimated energy/CO2 savings
Energy savings were estimated by comparing a standard cycle on a machine with heat exchanger to one without. Results in the dialysis unit showed 5.2 kWh vs. 4.7 kWh (with heat exchanger), a saving of 0.5 kWh per treatment, or approx. 10%.
However, electricity usage was almost 3x higher for a treatment at the home of a home-dialysing patient, where the incoming water temperature was 5C, as compared with 10-22C in the dialysis unit. Power consumption from the WRO and HD without heat exchanger was 14.05 kWh. Energy savings in this setting would be expected to be greater. Even a 10% saving would save 1.4kWh per treatment – 218.4kWh per year.
Actual savings to date
Initial recordings have been taken in the summer months with an incoming water temperature of approx. 18C. Under these conditions, retrofitting of the heat exchangers has reduced electricity consumption by 0.625kWh per treatment. For a typical patient on 3 treatments per week, if the energy saving remained constant, then total energy savings would be 0.625kWh x 3 x52 = 97.5 kWh. Carbon savings would be estimated as 97.5 x 0.58982* = 57.5 kg CO2e per year per machine, or 1.207 tonnes CO2e for all 21 machines.
However, energy savings are likely to increase in winter with lower water temperatures in patients' homes.
Additional Benefits
The 21 home dialysis patients will benefit from reduced electricity bills. This cost saving may in future be passed onto the renal service through a commensurate reduction in the financial support given towards patients' utility bills. At a standard domestic tariff of £0.16/kWh, the 0.625 kWh electricity saving equates to a cost saving of approx. 10p/ treatment, translating to £15.60/year per machine, or £327.60/year for all 21 machines. However, total energy consumption and energy savings from the heat exchangers are expected to increase in colder weather.
* GHG emission factor for electricity consumed (2010 grid rolling average), taken from 2012 Guidelines to Defra / DECC's GHG Conversion Factors for Company Reporting (Table 3c)
Details of Implementation
Following contact from the Green Nephrology programme, highlighting environmental and cost savings achieved by retrofit of heat exchangers in Kent, Dr Suren Kanagasundaram (Renal Consultant and Newcastle Green Nephrology Local Representative) asked the renal technicians to investigate the business case for retrofitting heat exchangers locally.
45 machines were found to be suitable for retrofit. Because of the greater energy savings in the home setting and the availability of funding via the home dialysis conversion budget, the decision was taken to prioritise retrofit of all 21 home machines.
The cost (approx. £4,700 (£223.70 per machine, including £7.50 labour costs)) was found from the home dialysis conversion budget.
Electricity energy saving in patients homes – with both environmental and financial benefits.
The project was shortlisted for the Green Nephrology Awards 2012. The PDF award entry poster may be downloaded from here.
Baling and Recycling of Bottles & Cardboard

By: Newcastle Upon Tyne Hospitals NHS Foundation Trust
£7,384 net savings (Actual)
85.2 tonnes CO2e (Estimated)
The Renal Unit produces huge amounts of waste plastic and cardboard during its clinical activities. In order to recycle this waste the Trust installed two new pieces of equipment. A cardboard baler was installed to service the whole Freeman Hospital site in March 2011, which allowed the Renal Unit’s cardboard to be baled and recycled. In November 2011 a smaller twin baler was also installed to crush and bale the segregated 5L acid bottles from each renal dialysis session. Cardboard and plastic bottle recycling has increased by over 90 tonnes and savings of over £7,000 have been achieved.
The project was initiated by consultant nephrologist, Dr Alison Brown, and modern matron, Julia Harding. Using the commitment shown by the renal department, the Trust Waste Officer was able to justify a business case and gain Executive approval.
Equipment comprises a Static Vertical Mill Sized Baler (MX600) on long term rental for cardboard, and a twin chamber compact baler (Compact 75) on two-year rental for dialysis 5L plastic bottles. Baled cardboard and bottles are collected by SITA UK (the Trust's general waste contractor).
Environmental Benefits
An estimated 12 tonnes of plastic bottle waste is produced by the renal department each year. Recycling all of this will save approximately 3.168 tonnes CO2e per year (1).
The renal unit has also been contributing its flattened cardboard to the main Freeman Hospital cardboard baler. Approximately 100 tonnes of cardboard waste is produced annually and recycling this saves an estimated 82 tonnes CO2e per year (2). Unfortunately we are not able to break this down to the specific amount of cardboard produced by the Renal Unit as all areas of the hospital feed into the main cardboard baler.
Total carbon savings from recycling of plastic and cardboard are therefore approximately 85.2 tonnes CO2e per year.
Importantly, recycling materials also reduces the need for virgin resources for new products. Although the benefits of this are hard to quantify, we know that increasing the recycling of resources instead of just disposing of them makes sense.
Furthermore, the compaction saves on CO2e emissions from large waste vehicle movements, since the much smaller volumes can be more easily stored and therefore collected less frequently.
(1)This is based on -230 kg CO2e per tonne of plastic recycled vs 34 kg CO2e per tonne of plastic sent to landfill (Annex 9, DEFRA 2011 Greenhouse Gas Conversion Factors for Company Reporting)
(2) This is based on -240 kg CO2e per tonne of cardboard recycled vs 580 kg CO2e per tonne of cardboard sent to landfill (Annex 9, DEFRA 2011 Greenhouse Gas Conversion Factors for Company Reporting)
Financial Benefits
The financial savings are summarised below:
|
Waste Type |
Predicted Annual Weight of Waste |
Previous Total Disposal Costs |
New Annual Baler Rental |
New Disposal Costs |
New Total Annual Costs |
Net costs |
|
Plastic Bottles |
12t |
£720 |
£1,456 |
-£540 |
£916 |
£196 |
|
Cardboard |
100t |
£6,000 |
£2,920 |
-£4,500 |
-£1,580 |
-£7,580 |
|
Totals |
112t |
£6,720 |
£4,376 |
-£5,040 |
-£664 |
-£7,384 |
To reduce the environmental impact and cost of waste disposal. The project was inspired by an early Green Nephrology case study: http://map.sustainablehealthcare.org.uk/heart-england-nhs-foundation-trust/diversion-waste-recycling-stream-through-use-baling-machines .
SITA UK (long term lease of cardboard baler; collection and rebate for baled cardboard and plastic). Local firm ATK Equipment (2-year lease of plastic bottle baler).
Sustained change has been maintained through positive reinforcement (telling staff and porters what we have saved so far by distributing graphs in our Green News and passing on information at team meetings) and regular visits by the Waste Officer to iron out any small issues. We plan to continue with the dissemination of regular update graphs to staff.
The project was the winner of the Green Nephrology Awards 2012; the award entry poster can be downloaded here.
£4,376 (annual rental costs for balers)
44:1 Haemodialysis Concentrate Solution

By: East Kent Hospitals University NHS Foundation Trust
Carbon savings from transport of smaller volumes of concentrate. In addition, using a 4.7ltr can rather than a 6ltr can will mean a reduction in manual handling effort for the renal unit staff transporting the concentrate solution from the store to machine. Also, a pallet holds 128 cans of 44 to 1 concentrate compared to 90 cans of the larger 34 to 1 concentrate can thus reducing the number of pallet movements and optimising storage area in the renal unit.
£0 (Actual)
16.22 tonnes (Estimated)
During haemodialysis, creation of the dialysate fluid requires a concentrated acidic solution of known constituents to be drawn into the machine. This solution is diluted with a set volume of purified water from a reverse osmosis unit to achieve the correct concentration. Our Trust had previously used cans of acidic concentrate which require a 34:1 ratio of dilution, i.e. 1 part concentrate to 34 parts water. This 34:1 solution is supplied in a 6 litre can. The same final composition can also be achieved using an alternative acidic solution with a concentration of 44:1 after some minor technical adjustments to the dialysis machine. This 44:1 solution can be supplied in a 4.7 litre can. The can size of each of the solution concentrations reflect a reasonable diluted volume to comfortably supply a 4-4.5 hour dialysis treatment.
Details of implementation
As the four most commonly used solutions were not available in the smaller container, the manufacturer BBraun was approached to develop the specific solutions with a 44:1 concentration in the required size container for the same cost and to provide advice on the minor technical changes needed to the dialysis machines.
The trust procurement and supplies department were consulted to arrange new product codes to be allocated to the new items when bulk ordering.
The dialysis machines’ settings were subsequently adjusted accordingly by the trust renal technicians to allow safe operation with the higher concentrations of solution.
The Higher concentration (44 to 1) solutions have been available for some time, although there are still a significant amount of treatments around the UK using the 34 to 1 can option. Switching to the 44 to 1 concentration cans is a relatively easy process at negligible cost and may be a more simple method of reducing concentrate solution storage without procuring and maintaining a more costly central acid delivery system.
Higher concentration dialysis solutions (44 to 1) are also available from other manufacturers and can be used in alternative brands of dialysis machine.
Benefits to environmental sustainability: Reduction in greenhouse gas emissions from road transport
The concentrate is manufactured and transported by road from Glandorf, Germany to Sheffield and from Sheffield to Kent. An estimate of the carbon savings from transporting smaller volumes can be made as follows:
Reduction of concentrate used per treatment = 6 to 4.7 litre can = 1.3 litres
Reduction of concentrate used daily in the Trust = 200 x 1.3 litres = 260 litres
Reduction of concentrate used annually = 260 x 312 days = 81,120 litres
Thus approximate weight each year = 81.1 tonnes
Glandorf to Sheffield = 960 km
Sheffield to Canterbury = 374 km
Total distance= 1334 km
Approximate annual reduction in greenhouse gas emissions from road freight:
= 0.14993 * x 81.1(tonnes) x 1334(km) = 16,220 kg CO2e / year = 16.22 tonnes CO2e / year
(* 2012 Guidelines to Defra/DECC's GHG Conversion Factors for Company Reporting (Annex 7, Table 7e))
This cost neutral initiative is primarily to reduce the burden to the environment in transporting dialysis consumables.
BBraun
Project entered to the Green Nephrology Awards 2012 - pdf poster available to download from http://sustainablehealthcare.org.uk/green-nephrology/resources/2012/09/green-nephrology-award-entries-2012-posters-g-n
Improved waste management in the Dialysis Unit Queen Margaret Hospital, Dunfermline

By: NHS Fife
£35,718 (Estimated)
56.3 tonnes CO2e (Estimated)
This case study builds on the Reducing Waste in the Dialysis Unit Queen Margaret Hospital, Dunfermline case study from April 2010 (http://map.sustainablehealthcare.org.uk/nhs-fife/reducing-waste-dialysis...).
A Green Nurse role was established to promote awareness and education on environmental issues in the workplace and minimize landfill waste and inappropriate clinical waste. A waste management hierarchy was developed using the following in order of preference:
REDUCE – reduce the amount of waste produced in the first place (most favoured)
REUSE – using materials repeatedly where possible
RECYCLE – send used materials to make new material for use
RECOVERY – recover energy for waste
LANDFILL – safe disposal into landfill sites (least favoured)
STEP 1: Waste segregation
A major finding from Waste Watch Weeks in 2009-10 was a lack of formalised waste management procedures pre and post dialysis treatments. 2.9kg of waste was generated per dialysis treatment (40.3 tonnes / year). At the start of 2010, 100% of this was sent as clinical waste for incineration. This has a particularly detrimental impact on the environment because of the very high temperatures at which clinical waste must be incinerated. By April 2010 we had reduced this incinerated waste from 100% to 31%, with 69% now being directed into the domestic waste stream because it was not contaminated eg packaging, bicarbonate bags etc.
STEP 2. Recycling
Next, a Domestic Waste Audit was carried out, which identified most of the waste was paper and plastic. We collaborated with Fife Council to divert as much of this as possible from landfill. Domestic waste bins ie black bags were removed from the clinical area and replaced with recycling bins and 83% of domestic waste is now recycled. Grade 7 plastic (saline bags and bicarbonate bags) still remain a challenge but we hope Fife Council will be able to take these soon. Education on environmental good practice is now included in our nurse education programme.
Financial Considerations
The creation of a ‘Green Nurse’ with protected time has been central to the success fo this project. Initial funding for this came via NHS Education for Scotland and the Scottish Renal Association. Fife Council provided recycling bins for free. Diverting clinical waste which is expensive to dispose of into the cheaper, domestic stream saved us £11,273 annually. Removing unnecessary consumables saved a further £24,900 annually. The cost for domestic waste disposal after recycling was £454.74 annually. Overall £35,718 annual saving.
Carbon Savings
Initially 72.5 tonnes CO2e was generated form the incineration of our clinical waste. Which was reduced to 22.5 tonnes CO2e a saving of 50 tonnes CO2e annually. After recycling, 4.7 tonnes of domestic waste was put into landfill. Assuming this was mostly grade 7 plastic, 14.8 tonnes CO2e would be generated by this (this is an over estimate as a proportion was kitchen waste). 23 tonnes of paper and plastic was recycled saving 21.1 tonnes CO2e giving an overall annual saving of 56.3 tonnes CO2e.
Queen Margaret Hospital, Whitefield Road, Dunfermline, Fife, KY12 0SU
The aim of the project was to promote awareness of environmental good practice by staff and reduce cost and carbon emissions with minimal impact on patient care.
(staff time: approx 4 hours per week from a dialysis nurse is spent on environmental awareness and practice.)
Bolus Administration of Intravenous Antibiotics

By: NHS Fife
In addition to the cost and carbon savings, benefits were gained by reducing the volume of fluid administered in the context of renal failure, more efficient use of nursing time and increased nurse-patient contact and IV cannula observation. Also time was not wasted locating infusion pump devices and the ward was quieter without bleeping pumps.
£17,060 (Estimated)
6.73 tonnes CO2e (Estimated)
Queen Margaret Hospital (QMH) has 24 in-patient beds, 20 dialysis stations and serves a population of 350,000. Prior to the end of 2010 all intravenous (IV) antibiotics were given by infusion even where bolus could be safely used. This used a great deal of plastic. Additionally semi-prepared ‘mini-bags’ (designed for use in the community) were being used for convenience which was unnecessary.
To determine if savings were possible a retrospective analysis of antibiotic use, cost and carbon emissions was performed based on pharmacy records over a one-year period (October 2009–September 2010). Savings were then calculated assuming a similar pattern of antibiotic use, price and nursing staff time, but assuming infusion is replaced by bolus administration. 13 antibiotics were identified as suitable for bolus administration after pharmacy review. Antibiotics requiring infusion were excluded from the analysis leaving a total of 6,175 doses infused. The financial and carbon saving (below) were large and steps were taken to change practice. Staff were educated to deliver drugs safely by bolus and a suitable preparation area was identified. Practice was changed from the beginning of 2011 with audit planned. This has been easily adopted by staff and there have been no safety concerns to date but maintining practice has been challenging.
Background
The NHS has an increasing chronic care burden and must conform to the NHS carbon reduction strategy in a time of relative funding reduction. Procurement forms a significant component of the NHS budget and 60% of the NHS carbon footprint. This rises to 72% for renal services where equipment and pharmaceutical use is high. Reducing procurement emissions is a ‘quick win’ and systematic analysis of clinical processes can identify non-essential consumables and provide opportunities to lean treatment pathways that will deliver both cost and carbon savings.
Financial Considerations
This project incurred no additional cost to the NHS being funded entirely by staff enthusiasm where extra work was required. All training could be provided ‘in-house’.
Excluding drug costs, infusion via an infusion pump cost £1.96 per administration (pump administration set, £1.38; 50-100mls sodium chloride or dextrose bag, £0.35; 20ml syringe, £0.09; 21G needle x2, £0.04; Alcowipes x2, £0.01) verses £0.22 for bolus administration (10ml syringe, £0.12; 10ml sodium chloride, £0.045; 21G needle x2, £0.04; Alcowipes x2, £0.01). The total cost, including ‘mini-bags’ was £11,158. Assuming identical antibiotic use the predicted annual cost saving was £9,830 (88.1%). Savings from reduced disposal (0.41 tonnes equipment waste saved) by incineration are estimated at £165 annually (assuming a cost of £400 per tonne) bringing the total saving to £9,995 per year. In addition to consumables, further annual drug cost savings of £7065.33 were made by purchasing vials for bolus administration rather than pre-prepared mini-bags for infusion bringing the overall total saving to £17,060 annually.
Carbon Savings
Supply chain emissions saved (manufacture, transport etc):
- Equipment: £9830 x 0.30 kg CO2e / £ * = 2949 kg CO2e
- Drug: £7065 x 0.43 kg CO2e / £ * = 3038 kg CO2e
Emissions saved from avoided incineration of plastic waste:
- 0.406 tonnes plastic x 1833 kg CO2e / tonne ** = 744 kg CO2e
Total emissions saved, per year:
- 2949 + 3038 + 744 = 10,020 kg CO2e, or 6.73 tonnes CO2e
* Greenhouse gas (GHG) conversion factors for supply chain were obtained from the 2012 Guidelines to Defra / DECC's GHG Conversion Factors for Company Reporting (Annex 13).
** Greenhouse gas (GHG) conversion factors for waste incineration were obtained from the 2011 Guidelines to Defra / DECC's GHG Conversion Factors for Company Reporting (Table 9d).
GETTING STARTED – ‘HOW TO’ GUIDE
- Ascertain current practice by auditing antibiotic use and administration methods on the ward – are you missing opportunities to reduce infusions?
- Involve senior nursing, medical and pharmacy staff early on.
- Patient safety is the first priority – confirm drugs which can safely be given by bolus and how this is done. Set out clear procudures that can be easily accessed in the preperation area.
- Identify an areas for bolus preparation if not already in existence.
- Listen to staff concerns and address these through education and training as needed.
- Ensure adequate numbers of trained staff are on the ward so that drugs can be administered as boluses on every shift.
- Set a start date which everyone is aware of.
- Measure the outcome by audit and staff feedback.
Further tips
Savings could be amplified if IV bolus administration was adopted as standard practice across NHS specialties and for all IV drugs suitable for this route of administration.
Queen Margaret Hospital, Whitefield Road, Dunfermline, Fife, KY12 0SU
The lead nurse for this project has since been asked by the Trust to extend the initiative to the Emergency Care Directorate (ECD). Her initial investigations show that in the ECD in 2011, 57,412 doses of IV antibiotics which could have been bolused were delivered by IVI, at a cost of £149,462. To change to bolus will save £138,554.
Central Delivery of Acid for Haemodialysis

By: Bradford Teaching Hospitals NHS Foundation Trust
Reduced acid wastage: only the actual acid required for any given treatment is ever used. Reduced solid waste: in 2008, 29,540 used canisters were disposed of as clinical waste. Saving on storage space and manual handling by nurses and porters: it is no longer necessary to transport 90 full canisters from ground- to first floor every day. Resilience to disruption of supply: the unit now has 3 weeks’ supply of solution at any one time.
£22,900 (Actual)
16.03 tonnes CO2e per year (Estimated)
The dialysis unit was previously supplied with 6 litre plastic cans of dialysate acid solution through weekly orders. These were delivered on pallets and could not be stacked to save on storage space.
The Problem:
1. Acid Wastage
As dialysis patients are prescribed different flow rates (either 800ml/min or 500ml/min) there is generally always an element of acid wastage. More so is this seen with patients on a 500ml/min dialysate flow with approximately 2.14 litres not used out of the 6 litre can per treatment. Throughout one year this equated to a total wastage to drain of 50,142 litres. When considering the total order for St Lukes was 147,700 litres for 2008, this amounted to a high percentage of waste.
2. Waste Disposal:
Empty canisters weighed approx. 143 grams and were disposed of via the clinical waste stream at a cost of £500 per ton. This amounted to an annual cost of approximately £2,363 per year.
The Solution:
In 2009, the renal technicians proposed a move to central acid delivery. This is acid delivered to a dialysis unit in bulk load through fortnightly/monthly deliveries and pumped into holding tanks (delivery frequency depends on the size of holding tanks installed). This acid is then distributed to all dialysis machines via a piped loop system with outlets at each dialysis station. They noted that all the dialysis machines in use had the capability to be retrofitted with central delivery acid systems at minimal expense.
The new two-acid, two-loop system was installed in 2011, at a cost of £40,000. This comprises a 7000 litre storage tank for the main acid solution, a 4000 litre tank for the low calcium solution, and a pressurised loop to deliver the acid to the dialysis machines. The Trust also paid an additional £3,900 for enabling works – a bund system connected to an outside drain, in case of leakage.
Benefits to the environmental sustainability of kidney care (section updated November 2012)
1. Reduced Acid Wastage
Using 6 litre cannisters, the average acid wastage per dialysis session for a patient on a 500ml/min flow rate was 2.14 litres. Throughout one year this equated to a total wastage to drain of 50,142 litres.
At £0.38/ litre, the predicted savings were £19,054 exc. VAT per year. Actual savings achieved were £19,372 per year.
Multiplying this cost saving by the emissions factor for pharmaceuticals (2012 Guidelines to Defra / DECC's GHG Conversion Factors for Company Reporting, Annex 13) produces an estimate of carbon savings from avoided supply chain activities: 0.43 x 19,372 = 8,330 kg CO2e per year
2. Reduction in packaging waste
29540 empty canisters were previously disposed of per year (in 2008), each weighing 142.6 grams, amounting to 4.2 tonnes of plastic waste per year. The carbon savings from avoiding disposal of this waste via the clinical waste stream can be estimated at
4.2 x 1,833 (life-cycle GHG emissions factor for incineration)* = 7,699 kg CO2e
* DEFRA emissions factors for incineration do not specifically account for clinical waste, which is commonly undertaken at higher temperatures. To reflect the increased emissions that are likely to result from the incineration of clinical waste, the highest available emissions factor for incineration was applied (Table 9d, 2011 Guidelines to Defra / DECC's GHG Conversion Factors for Company Reporting)
[Combined savings = 16.03 tonnes CO2e per year]
Financial appraisal
Investment: £40,000 for storage tanks and piping; £3,900 for enabling works. Total: £43,900.
Actual savings: £19,372 per year from reduced acid wastage; £3,700 from reduced waste disposal. Total: £23,072 per year.
Return on investment at 5 years:
((Total saving to date - total cost to date) / (total cost to date)) * 100
((£23,072 * 5 - £43,900)/£43,900) * 100 = 163%
Renal Dialysis Unit, St Luke's Hospital, Bradford
To reduce acid wastage, packaging and money
Support from the Bradford Green Nephrology Local Representative, Dr John Stoves (consultant nephrologist)
Report published in the Trust newsletter ("Trust Today" March 2011, p8). Green Nephrology Awards 2012 - award entry poster available to download from http://sustainablehealthcare.org.uk/green-nephrology/resources/2012/09/green-nephrology-award-entries-2012-posters-d
Waste Management in the Renal Dialysis Unit - Case Study & How-to Guide

By: NHS Greater Glasgow and Clyde
£15,567 (Estimated)
85 tonnes CO2e (Estimated)
Within NHS Greater Glasgow and Clyde (GGC) 505 people attend our chronic hospital haemodialysis programme equating to 78,780 resource intensive treatments per year in six renal dialysis units (RDUs). We targetted clinical waste and unnecessary consumable equipment use as a simple and efficient method of reducing green house gas emissions (GHG) without impacting on the number or quality of dialysis treatments. Our health board already has off-site recycling of nearly 100% it’s domestic waste, so unlike many units we do not need to recycle at source. We focused on diverting wasteaway from expensive incineration and into the domestic waste stream for recycling. Environmental representatives for each of the units were asked to audit current equipment use per dialysis session for both fistula and line users and indentify possible areas of environmental saving in their unit. We then met as a group including senior nursing and medical representatives to agree which changes to make.
Areas of change identified included: Disposal of bicarbonate cartridges into domestic waste, segregation of domestic waste into black bags versus all waste into clinical waste bags as was prior practice, potential for reduction of Griff Bins® and online priming to reduce Saline bags.
Background
The NHS generates 25% of the UK’s public sector GHGs. Legislation now requires drastic cuts in NHS emissions of 80% by 2050. While GHG emissions from procurement including waste, account for 52% of the NHS Scotland total, in renal services, where consumable equipment use is high, this rises to 72% with waste comprising 9.6% and medical equipment 25% of overall emissions. For frequent treatments such as haemodialysis, small environmental and cost savings per treatment can translate into much larger savings overall.
Intended benefits
Benefits to patients:
Dialysis patients are not only more susceptible to climate change (CC) effects such as heat waves and transport disruption, but they rely on the continued supply of drugs and disposable equipment. Reducing GHG emissions now will mitigate the effects of CC and reduce the financial burden associated with renal dialysis allowing redirection of funds into other areas of patient care including the predicted expansion of renal dialysis within our region.
Benefits to staff:
The use of a network of ground level representatives promotes good environmental practice at work and also engages staff in implementing change through quantifying savings directly attributable to their actions.
Benefits to the organisation:
In addition to cost and environmental savings for renal services, this project will contribute to institutional change by promoting lower carbon care on six acute hospital sites. Translating corporate environmental policies into operational practice remains a challenge for the NHS. The approach of using operational level networks of representatives to maintain and promote good environmental practice will generate lasting change and can be adapted to other high resource areas within NHS GGC such as theatres, ITUs and day case procedure areas with large potential savings.
Possible disadvantages
Any potential effects on health and safety, infection control and porter services should be considered and discussed with the relevant departments as needed. No significant problems identified to date, although there is some resistance to getting rid of Griff Bins. Currently this is getting taken up at higher management levels to try and resolve.
What barriers might be encountered when introducing a waste management programme?
All staff contacted were enthusiastic and keen to be able to contribute to reducing GHG emissions. No doubt the challenge will be maintaining good environmental practice in the longer term. The presence of local represenatives in each unit will help to sustain this change together with an ongoing audit process.
Financial Considerations
These changes have been free to implement and have been funded entirely by the good nature and enthusiasm of NHS staff.
Cost and Carbon Savings
Approximately 85 tonnes CO2e and £15,567 annually can be saved across all six RDUs (NOT includine reduced expenditure on unnecessary equipment, such as saline bags). Additionally, five sites use 1.7kg polyethylene Griff Bins® rather than orange clinical waste bags. By reverting to standard clinical waste bags (approximately 14,000 bins saved), 43 tonnes CO2e and £92,832 could be saved annually (£84,000 from purchasing and £8,592 from incineration costs). These estimates do not include supply chain emissions, i.e. those generated from the manufacture and transport of the product to the RDU.
Method of CO2e calculation:
- The CO2e emission conversion factor for the incineration of clinical waste has been taken as 1.8 tonnes CO2e per tonne clinical waste * however higher conversion factors exist. These can double CO2e estimates.
- The CO2e does not include domestic waste figures, which does increase in weight, due to uncertainty surrounding an appropriate conversion factor in our case. NHS GGC has an exemplary domestic waste policy with the majority of waste recycled. So it may represent a net CO2e saving, however further information is required before this calculation can be included.
* Reference: The Carbon Footprint of a Renal Service in the United Kingdom. Connor A, Lillywhite R, Cooke MW. Quarterly Journal of Medicine Advance Access published online on August 18, 2010
Major Risks
Patient Safety
Only non-contaminated waste was diverted into the domestic waste stream so there was no adverse impact on patient safety.
Financial Risks
None identified.
GETTING STARTED – ‘HOW TO’ GUIDE
- Set up the working group:
- Identify waste management representatives from each RDU to promote, sustain and develop an efficient waste management system as part of a coordinated waste management project within NHSGGC renal services.
- Engage senior stakeholders to support the project including senior nursing and medical staff, Renal Services management team, the Education and Practice Development Nurse for Renal Services, the Estates department and the Sustainability Officer for NHS GGC.
- Adapt for your area eg Glasgow already recycles all domestic waste off site, so no need to waste time and money doing this again.
- Focus on “quick wins” to reduce clinical waste by diverting it into the domestic waste stream:
- Use the Green Nephrology Programme as a model of good environmental practice and existing models of a successful waste management eg Queen Margaret Renal Unit, Fife, £36k annually and received 3rd place in the Innovation in Renal Medicine Awards 2011.
- Audit current patterns of consumable equipment use and disposal.
- Identify safe opportunities for reducing clinical waste (uncontaminated material does not need to be incinerated via the clinical waste stream).
- Identify equipment that could be safely removed from the dialysis process.
- Estimate potential financial and GHG emission savings, expressed as carbon dioxide equivalents (CO2e), by weighing clinical and domestic waste from two dialysis sessions (using AV fistula and catheter methods) before and after planned waste reduction and estimating the change in weight overall and emission factor. (Additionally, where unnecessary use of equipment has been discontinued, savings in supply chain emissions may be roughly estimated by multiplying avoided expenditure by the DECC GHG conversion factor* for the medical equipment industry.) *see “The 2009 Guidelines to Defra / DECC's GHG Conversion Factors for Company Reporting, Annex 13
- Consider potential health and safety or infection control issues identified and raise these with these departments as appropriate.
- Implement change and determine the actual cost and environmental savings by auditing total daily waste produced over a period of time before and after waste reduction.
- Repeat the audit after six months to ensure change is maintained.
- Consider extending to inpatient dialysis treatments.
- Look for additional opportunities such as reducing clinical waste for inpatient biopsy or central line procedures.
Further tips
Think of everyone who may be affected by your changes outside your unit eg Hospital Porters if you are changing the type or amount of waste for removal. Talk to these groups first to avoid problems later.
FURTHER INFORMATION & SUPPORT – PLEASE CONTACT:
Pamela Sinclair pamela.sinclair@ggc.scot.nhs.uk
Tara Collidge tara.collidge@nhs.net
Project located across all six renal units in NHS Greater Glasgow and Clyde
Support received via the Green Nephrology Network: http://sustainablehealthcare.org.uk/green-nephrology
